Acute vs. Chronic Kidney Disease: Know the Difference
When it comes to kidney health, two terms often arise—Acute Kidney Injury (AKI) and Chronic Kidney Disease (CKD). While both affect kidney function, their causes, symptoms, duration, and treatment vary greatly. Understanding the Acute vs Chronic Kidney Disease is essential for early detection, proper treatment, and long-term kidney care.
In this comprehensive guide, we will explore the fundamental distinctions between these two conditions to help you stay informed and proactive about your kidney health

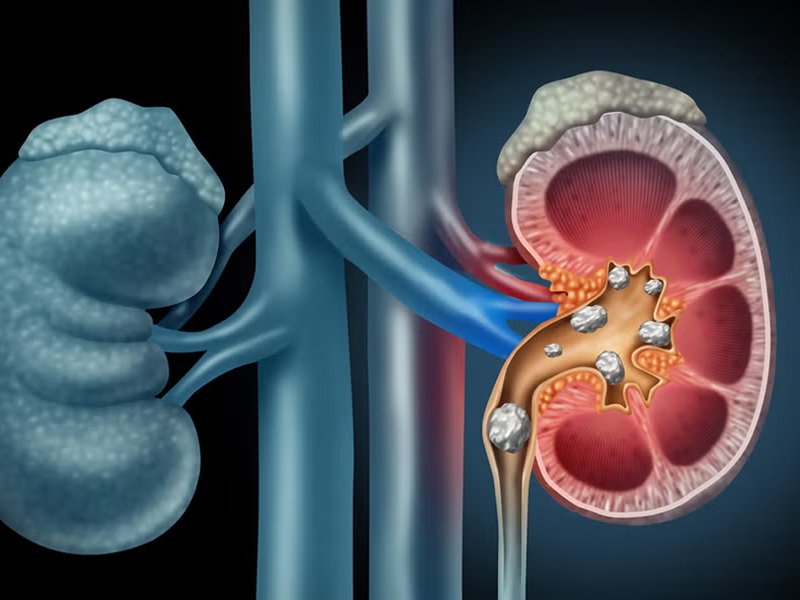
🚨 What Are Your Kidneys and Why Are They Important?
Before diving into the differences, it’s important to understand the role of your kidneys.
Your kidneys:
- Filter 50 gallons of blood every day
- Remove waste and extra fluid through urine
- Balance electrolytes (like sodium and potassium)
- Control blood pressure
- Produce hormones that regulate red blood cell production
Damage to the kidneys—whether sudden or long-term—can lead to severe health problems, and in some cases, be life-threatening Acute vs Chronic Kidney Disease.
⚡ What is Acute Kidney Injury (AKI)?
AKI (also called Acute Renal Failure) refers to a sudden loss of kidney function over a few hours or days.
🔍 Causes of AKI:
- Severe dehydration
- Sepsis or infections
- Major surgery or trauma
- Heart failure
- Certain medications (NSAIDs, antibiotics, contrast dyes)
- Blockage in urinary tract (kidney stones, enlarged prostate)
⚠️ Symptoms of AKI:
- Sudden decrease in urine output
- Swelling in legs, ankles, or around eyes
- Fatigue or confusion
- Nausea or vomiting
- Shortness of breath
- High blood pressure
🧪 Diagnosis:
AKI is diagnosed through:
- Blood tests (elevated creatinine levels)
- Urine output measurement
- Ultrasounds or CT scans to identify blockages
💉 Treatment:
- Treat underlying cause (e.g., infection or blockage)
- Hydration with IV fluids
- Medications to manage potassium levels or fluid overload
- Temporary dialysis in severe cases
Good news: AKI is often reversible if treated promptly
🕒 What is Chronic Kidney Disease (CKD)?
CKD is a long-term, progressive loss of kidney function over months or years. Often referred to as a “silent killer,” it may not show symptoms until significant damage has occurred.
🔍 Causes of CKD:
- Diabetes (Type 1 & 2)
- High blood pressure (Hypertension)
- Polycystic kidney disease
- Glomerulonephritis (inflammation of filtering units)
- Long-term use of certain medications
Recurrent kidney infections
⚠️ Symptoms of CKD:
In early stages, CKD may have no noticeable symptoms. As it progresses, patients may experience:
- Persistent fatigue
- Swollen feet or hands
- Foamy or bloody urine
- Loss of appetite
- High blood pressure
- Muscle cramps
- Darkened skin
- Trouble concentrating
🧪 Diagnosis:
CKD is staged from 1 to 5 based on the eGFR (estimated Glomerular Filtration Rate):
- Stage 1: Normal kidney function but signs of damage
- Stage 2-3: Mild to moderate loss of function
- Stage 4: Severe damage
- Stage 5: Kidney failure (requires dialysis or transplant)
Tests include:
- Serum creatinine
- eGFR
- Urinalysis (for protein or blood)
- Ultrasound or CT scan
💊 Treatment:
- Lifestyle modifications: low-sodium diet, regular exercise
- Blood sugar & pressure control
- ACE inhibitors or ARBs
- Avoidance of nephrotoxic medications
- Dialysis or transplant at stage 5
Note: CKD is not reversible, but its progression can be slowed with proper care.
🔬 Acute vs. Chronic Kidney Disease: Comparison Chart
Feature
Onset
Reversibility
Causes
Symptoms
Diagnosis
Duration
Treatment Focus
Dialysis
Acute Kidney Injury (AKI)
Sudden (hours to days)
Often reversible
Dehydration, infection, surgery
Rapid and severe
Sudden rise in creatinine, low urine
Short-term (if treated)
Treat the cause quickly
Sometimes temporary
Chronic Kidney Disease
Gradual (months to years)
Irreversible
Diabetes, hypertension, genetic disorders
Often asymptomatic early
eGFR < 60 for 3+ months
Long-term or lifelong
Slow disease progression
May require long-term dialysis or transplant
🩺 Importance of Early Detection
Many people discover kidney disease too late. That’s why regular health checkups and blood pressure or diabetes management are essential—especially if you have risk factors.
Ask your doctor about:
- Creatinine and eGFR tests
- Urinalysis (to check for protein)
- Blood sugar levels
- Blood pressure readings
Prevention Tips for Kidney Health
✅ Stay Hydrated Drink enough water daily, especially in hot climates or if you're active.
✅ Manage Diabetes and Blood Pressure Follow medical advice strictly and take prescribed medication.
✅ Avoid Overuse of NSAIDs Painkillers like ibuprofen and diclofenac can harm your kidneys.
✅ Eat a Kidney-Friendly Diet • Low in salt, processed foods, and sugar • Rich in fruits, veggies, and lean protein
✅ Quit Smoking and Limit Alcohol
✅ Regular Screening If you're over 40 or have a family history, get tested annually
🧘 Real-Life Impact: A Patient’s Story
Ramesh, a 58-year-old diabetic, ignored swelling in his legs for months. What he thought was just “age catching up” turned out to be Stage 4 CKD. Early lifestyle changes could have slowed his kidney decline. His story is a powerful reminder that awareness can save lives